Photograph by Moredun Animal Health Ltd/Science Photo Library
A scanning electron micrograph provides a color depiction of a small cancerous tumor within a human lung. The tumor is covered in microscopic hairlike structures called microvilli, which enable absorption and secretion. Smoking and other tobacco use are responsible for nearly all cases of lung cancer.
Cancer is a disease that begins as a renegade human cell over which the body has lost control. In order for the body and its organs to function properly, cell growth needs to be strictly regulated. Cancer cells, however, continue to divide and multiply at their own speed, forming abnormal lumps, or tumors. An estimated 6.7 million people currently die from cancer every year.
Not all cancers are natural-born killers. Some tumors are referred to as benign because they don't spread elsewhere in the body. But cells of malignant tumors do invade other tissues and will continue to spread if left untreated, often leading to secondary cancers.
Cancers can start in almost any body cell, due to damage or defects in genes involved in cell division. Mutations build up over time, which is why people tend to develop cancer later in life. What actually triggers these cell changes remains unclear, but diet, lifestyle, viral infections, exposure to radiation or harmful chemicals, and inherited genes are among factors thought to affect a person's risk of cancer.
Lung cancer is the world's most killing cancer. It claims about 1.2 million victims a year. Most of those victims are smokers, who inhale cancer-causing substances called carcinogens with every puff. Experts say around 90 percent of lung cancer cases are due to tobacco smoking.
Breast cancer now accounts for almost one in four cancers diagnosed in women. Studies suggest the genes you inherit can affect the chances of developing the illness. A woman with an affected mother or sister is about twice as likely to develop breast cancer as a woman with no family history of the disease. Lifestyle may also have an influence, particularly in Western countries where many women are having children later. Women who first give birth after the age of 30 are thought to have a three times greater risk of breast cancer than those who became mothers in their teens.
Geographical Distinctions
There are also stark geographic differences, with incidence rates varying by as much as thirtyfold between regions. In much of Asia and South and Central America, for example, cervix cancer is the most deadly in females. However, in North America and Europe another kind of gynecological cancer, ovarian cancer, is a more serious threat.
Among males, southern and eastern Africa record the second and third highest rates of oesophageal, or gullet, cancer after China, but western and central regions of Africa have the lowest incidence in the world. Differences in diet may explain this.
Nevertheless, the reasons why many cancers develop remain elusive. Brain cancer, leukemia (blood cancer), and lymphoma (cancer of the lymph glands) are among types that still mystify scientists.
Treatments
Yet ever more people are surviving diagnosis thanks to earlier detection, better screening, and improved treatments. The three main treatment options are surgery, radiotherapy and chemotherapy. Radiotherapy, also called radiation therapy, involves blasting tumors with high-energy x-rays to shrink them and destroy cancerous cells. Chemotherapy employs cancer-killing drugs.
Even so, future cancer cases are predicted to climb, since the world's population is aging. The proportion of people over age 60 is expected to more than double by 2050, rising from 10 percent to 22 percent. This will add an estimated 4.7 million to the cancer death toll by 2030.
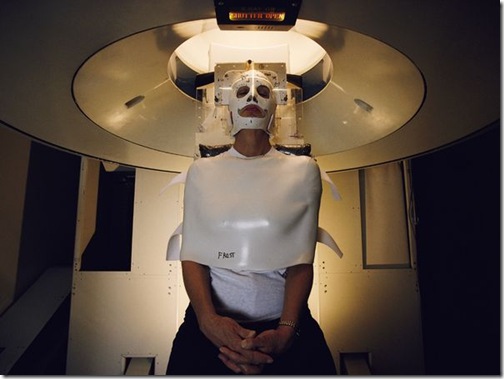
Radiation Treatment
Photograph by Karen Kasmauski
For Bonnie Frost, radiation offers hope in her fight against cancer. At the University of California's Lawrence Berkeley Laboratory, doctors pinpoint the tumor pressing against her spinal cord with a CT scanner, then treat it with heavy-ion radiation. The mask and brace keep her head perfectly still.
Source: http://science.nationalgeographic.com/science/health-and-human-body/human-diseases/cancer-article/